So after mindo and mobility, there is only one M left: masks.
I looked at this previously, but the “expert opinion” that masks lowered Japan’s Covid burden early in the pandemic is clearly wrong for three reasons.
1) The Japanese were far from universally masked prior to the first state of emergency in April 2020. I think these photos of the Japanese people’s political representatives in late March 2020 are pretty, er, representative of mask-wearing in Japanese workplaces at the time.
Bear in mind that this is about two weeks after the Czech Republic became the first European country to mandate masks. Moreover, Hunter et al. found requirements/recommendations for masks in public spaces in Europe in March/April 2020 were associated with an increase in the incidence of infections.
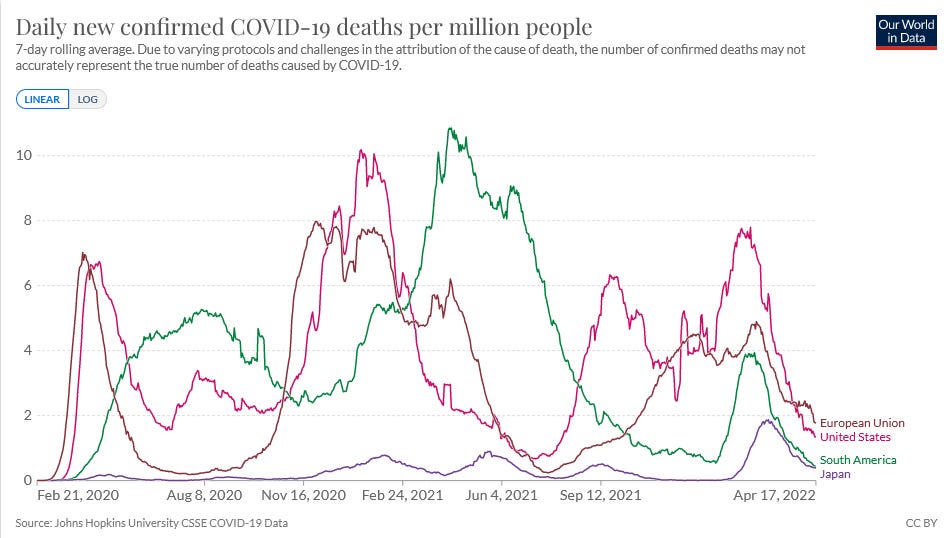
2) Even after universal masking was adopted in much of Europe and the Americas, the mortality gap didn’t narrow.
3) Most importantly, there’s no good evidence that masks lower the risk of respiratory infections.
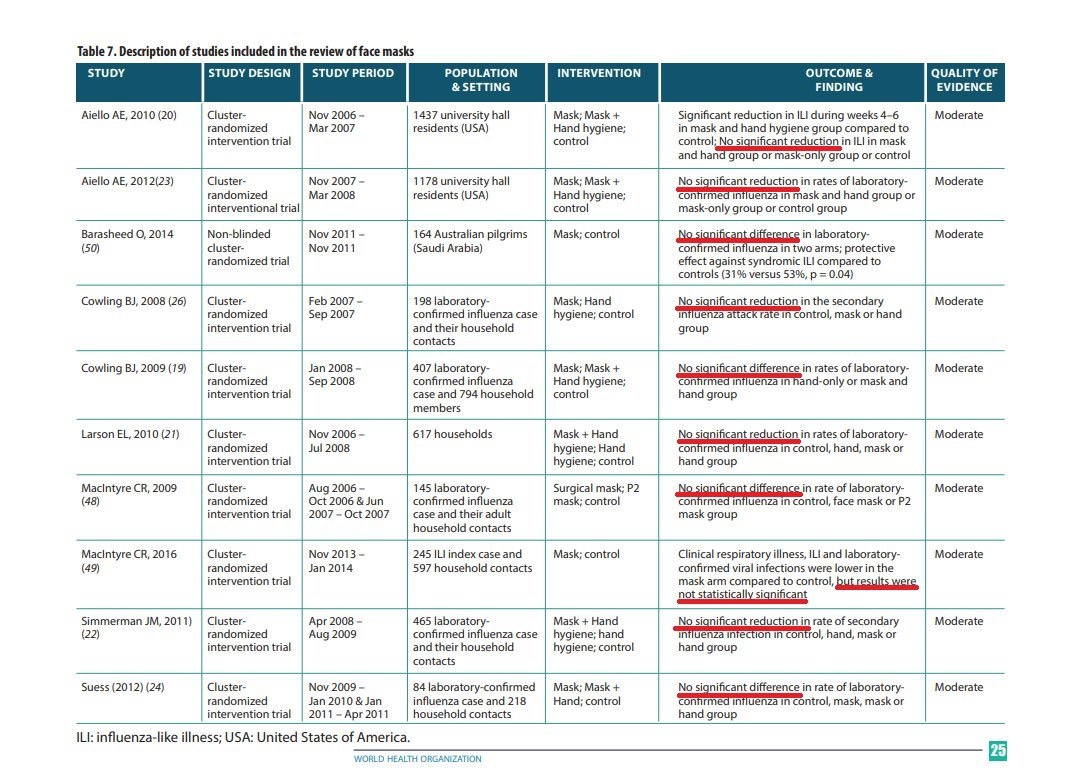
The one pre-Covid cluster randomised controlled trial (RCT) of masks in Japan to prevent colds had the same result as the 10 RCTs of masks to prevent influenza reviewed by the WHO in 2019 (pictured), one RCT done in France during Swine Flu, the one RCT done in Denmark for Covid, and a 6000-person cluster RCT done in Saudi Arabia for cold and flu viruses: no significant difference between the mask wearers and controls.
As for the mask-promotion cluster RCT in Bangladesh, even if you’re willing to overlook the numerous methodological defects pointed out by Gato El Malo here and here, the tiny risk reduction in the original study disappeared upon reanalysis when considering the statistical sampling biases.

Then we have Covid-era studies that found no effect of mask mandates on infections in schools in Florida, Spain, Finland, and Wales, and a study that found no effect of mask mandates or usage rates on case growth in the US.
And a study from Canada clarified the reason: cloth masks, surgical masks, and KN95 masks with a 3-mm gap only filter 10% of the aerosol particles that carry virus.

In fact, the Japanese media was honest about masks in December 2019…
Why masks can’t prevent influenza
… and even as late as early April 2020.
Are cloth masks effective? WHO says “They aren’t recommend whatever the circumstances”
That article even mentions the cluster RCT in Vietnamese hospitals that found significantly higher rates of influenza-like illness (ILI) in staff who wore cloth masks.
However, the refusal of Japan politicians, media, and “experts” to even acknowledge the above data and the religious conviction that masks saved Japan from a fate worse than New York mean that whenever cases in Japan rise, the solution is masks while dining (as mandated in Osaka)…
…masks in the pool…
…masks during sports (as requested in Yamanashi)…
masks, masks, masks!
So if it wasn’t the 3 Ms, what does explain Japan’s low Covid death count? We’ll look at possible reasons in the next post.
Update 25/4/2022
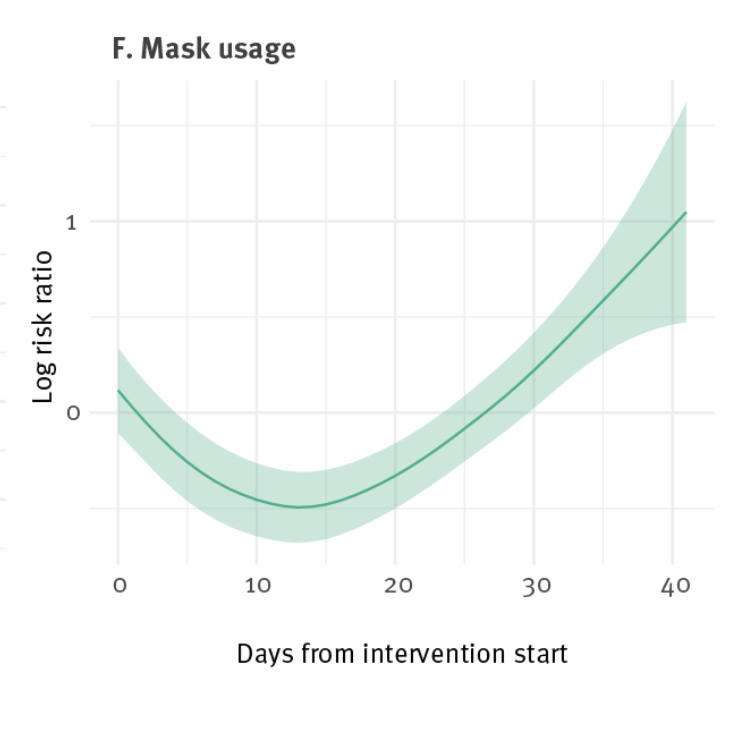
In case the studies cited above weren’t enough, a study of 35 European countries over the 2020/2021 autumn/winter wave has just been published that found reported mask usage had a positive correlation with Covid deaths per capita (i.e., countries with higher mask usage had higher Covid mortality rates).
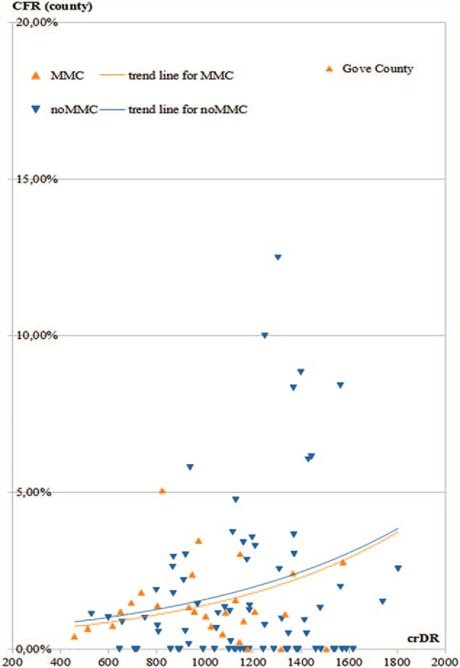
And another study finds that mask mandates were associated with higher case fatality rates in Kansas.
Update 2/6/2022
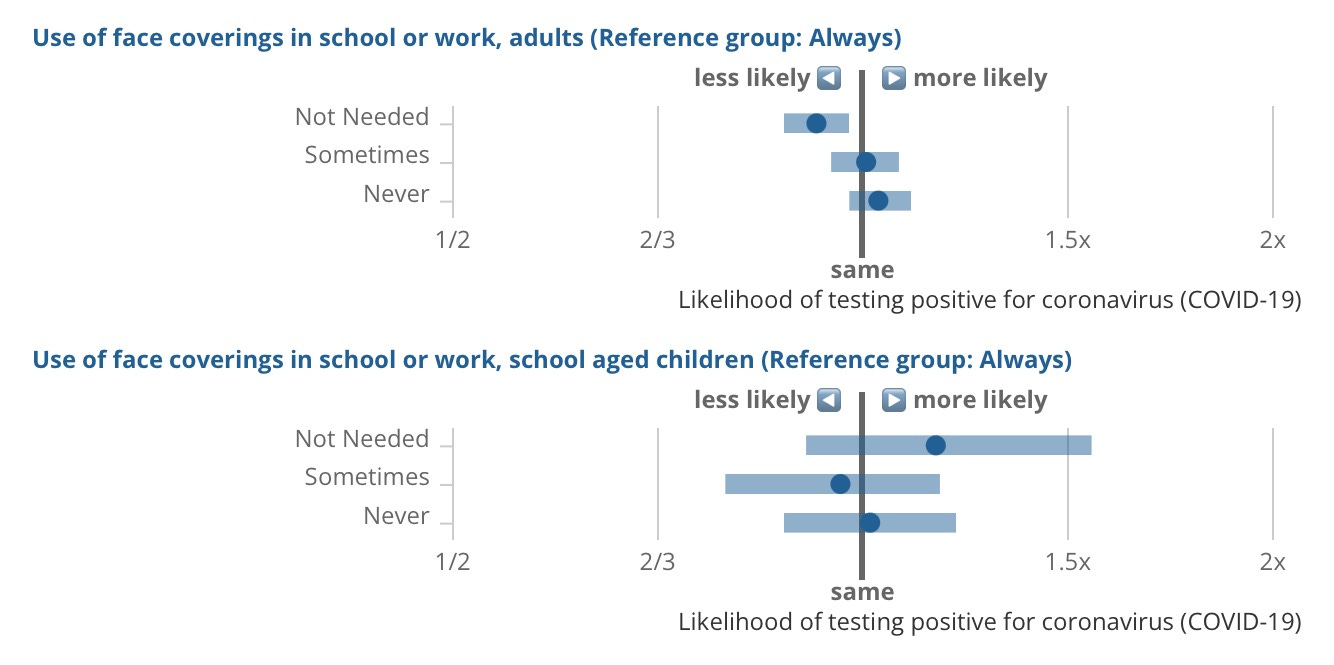
Let’s add a few more studies to the list. First, here are the results of a survey by the U.K.’s Office of National Statistics. There were no differences in infection rates among adults and children who did/didn’t wear masks at school or work.
Next we have a failed replication (or debunking) of a garbage CDC study. In short, school mask mandates made no difference to pediatric cases rates in America.
And lastly (for now), a new peer-reviewed study of 169 countries finds mask requirements (and 9 other NPIs) didn’t reduce Covid deaths.
Update 2 July
A new study has come out showing no difference in student case rates in two adjoining school districts in North Dakota: one with a mask mandate (Fargo) and one without (West Fargo). It’s getting a bit to predictable now, isn’t it?
Update 1 September 2022
In an international survey of 18,497 people who declined to take the Covid jabs, “those who reported never wearing a mask or face covering, consistently reported the lowest incidence of COVID-19 symptoms.”
Update 29 September 2022
A 21-study meta analysis finds “no statistically significant difference in respirator or surgical mask effectiveness in preventing SARS-CoV-2 infection (OR 0.85, [95%CI 0.72, 1.01]).”
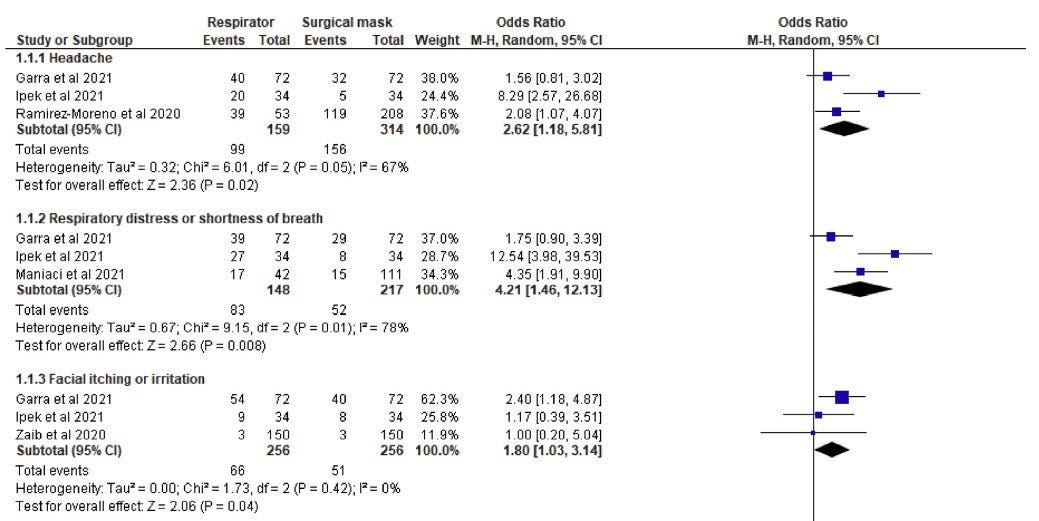
On the other hand, “Healthcare workers experienced significantly more headaches (OR 2.62, [95%CI 1.18, 5.81]), respiratory distress (OR 4.21, [95%CI 1.46, 12.13]), facial irritation (OR 1.80, [95%CI 1.03, 3.14]) and pressure-related injuries (OR 4.39, [95%CI 2.37, 8.15]) when wearing respirators compared to surgical masks.”
Update 12 October 2022
A study from Spain found no association between mask use and infection risk among close contacts.
Another study found “no reduction in per-population daily mortality, hospital bed, ICU bed, or ventilator occupancy of COVID-19-positive patients attributable to the implementation of a mask-wearing mandate” in Bexar County, Texas.
A study by the CDC, of all places, found no difference in reported mask use among positive Covid cases and negative controls.
Finally for now, a study found no association between infection rates and mask use during sports among high-school athletes in Wisconsin. Quick, someone tell the governor of Yamanashi!
Update 30 November 2022
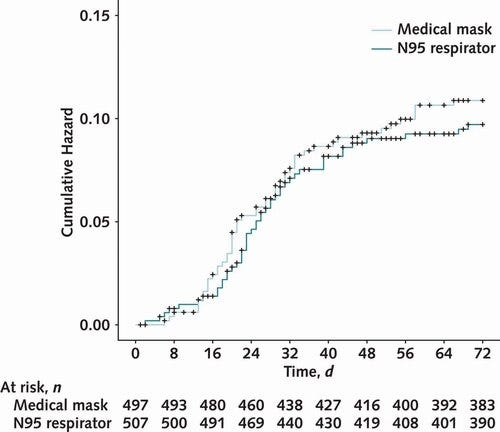
A randomised trial of surgical masks and N95 masks involving over 1000 healthcare workers in four countries found no significant difference in infection rates.
Adverse events were slightly higher in the N95 arm: 10.8% vs 13.6%.
Update 30 January 2023
A paper looking at the effectiveness of NPIs in France between March 2020 and January 2021 found the following results for mask mandates.
The most homogeneous NPI in terms of correlation coefficient remained mask wearing (without, however, exhibiting a strong correlation): for instance, mandatory mask wearing in public transit was slightly negatively correlated with both COVID-19 ICU admissions (-0,16) and viral reproduction rate (-0.22), but not significantly with COVID-19 hospitalizations (-0.05). An even smaller effect was observed regarding the mandatory wearing of masks in indoors public venues, with minimally-significant negative correlation with viral reproduction rate (-0.10), and no significant correlation with either COVID-19 ICU admissions (-0.02) nor hospitalizations (0.02). Even less convincing results were found regarding the correlation of mandatory mask wearing at the workplace, with a borderline insignificant negative correlation with viral reproduction rate (-0.10), no significant correlation with COVID-19 ICU admissions (0.08), and even slightly positive correlation with to COVID-19 hospitalizations (0.13).
Update 2 February 2023
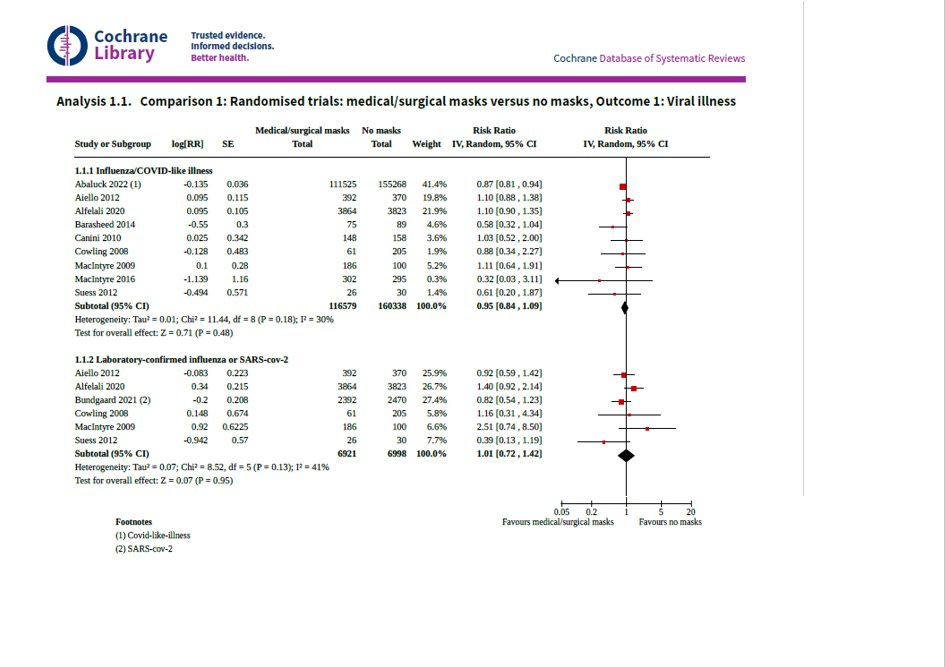
A Cochrane meta-analysis looking at 12 RCTs finds the following.
Wearing masks in the community probably makes little or no difference to the outcome of influenza‐like illness (ILI)/COVID‐19 like illness compared to not wearing masks (risk ratio (RR) 0.95, 95% confidence interval (CI) 0.84 to 1.09; 9 trials, 276,917 participants; moderate‐certainty evidence. Wearing masks in the community probably makes little or no difference to the outcome of laboratory‐confirmed influenza/SARS‐CoV‐2 compared to not wearing masks (RR 1.01, 95% CI 0.72 to 1.42; 6 trials, 13,919 participants; moderate‐certainty evidence).
A study looking at Covid hospitalisations and deaths in the USA after states reopened their economies “did not find significant differences in the change in hospitalization trend associated with reopening between states with and without a mask mandate at the time of reopening.”
Update 7 April 2023
A new study finds the lifting of mask mandates at a large London hospital during the first 10 months of Omicron (Dec 2021- Sept 2022) had no discernible effect on hospital-acquired Covid cases.
Update 7 August 2023
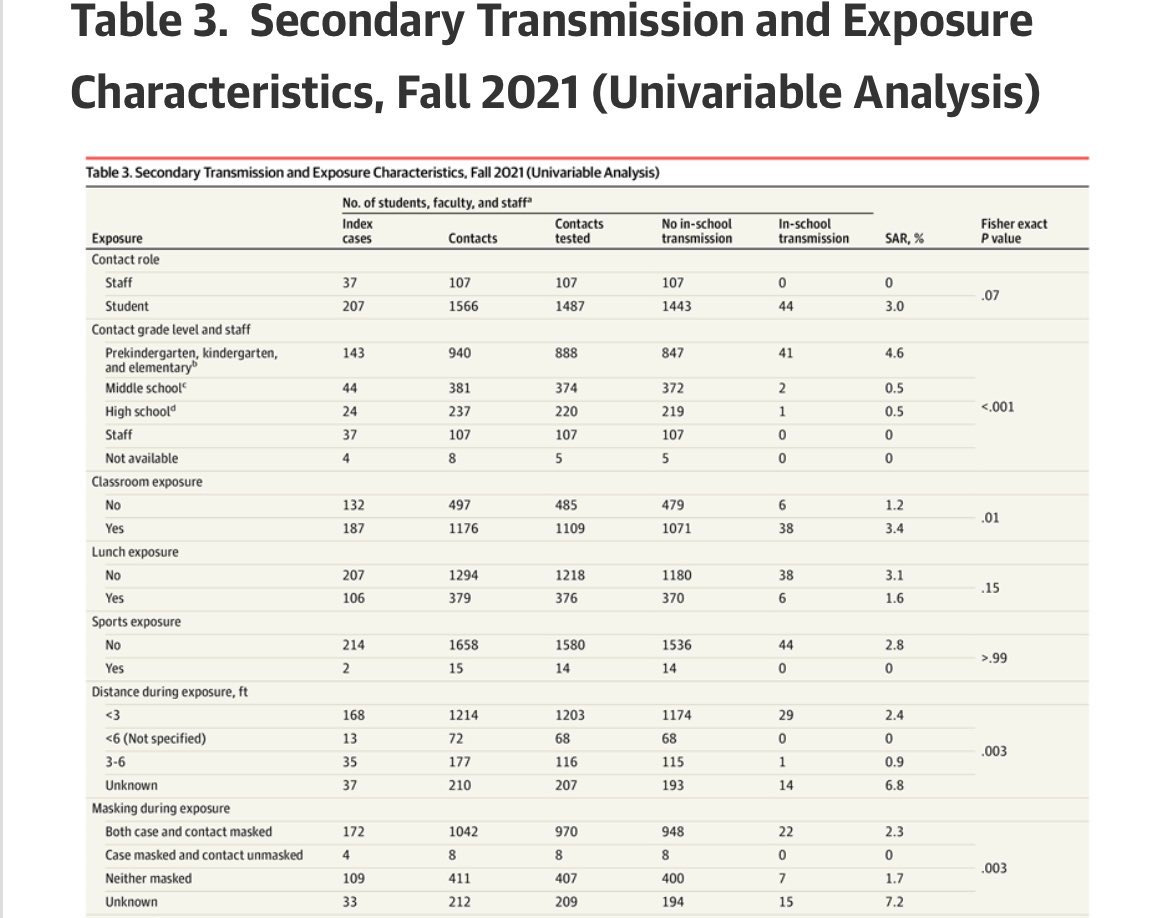
A study of in-school transmission during the Delta wave in Massachusetts finds that cases infected contacts 2.3% of the time when both were masked but only 1.7% of the time when both were unmasked. Your mask infects me; my mask infects you!
Staying in Massachusetts, another study debunks a widely-cited NEJM article by increasing the dataset and time period and accounting for prior infection: “We failed to find a notable change in student cases in mask mandate districts compared with the 70 districts in the original study (-0.08/1000; p=0.98) and found a slight increase compared with a statewide control group +3.63/1000 (p=0.291). Results were similar for students and staff combined. Districts that dropped mask mandates first experienced the largest decreases in cases (22% drop vs 12% in the masked districts).”